| Age and gender | Usually younger age group 30 - 50 years, median age 58 years, slight female preponderance (M/F: 1:1.014) [12, 13] | Mean age: 55 - 60 years, male/female: 1:1.35 [1] |
| Clinical presentation | Usually silent in retroperitoneal variety till adjacent structures are compressed | Intra-luminal tumors erode mucosa often present as GI bleed, bowel dilatation, vomiting, exophytic tumors may be silent clinically till necrosis and fistula formation occurs |
| Location | Omentum, mesentery, liver, pancreas, pelvis (80%), retroperitoneum (20%) [14] | Gastrointestinal tract from esophagus to anus (mc. in stomach (60-70%) followed by small bowel (20-30%) [4] |
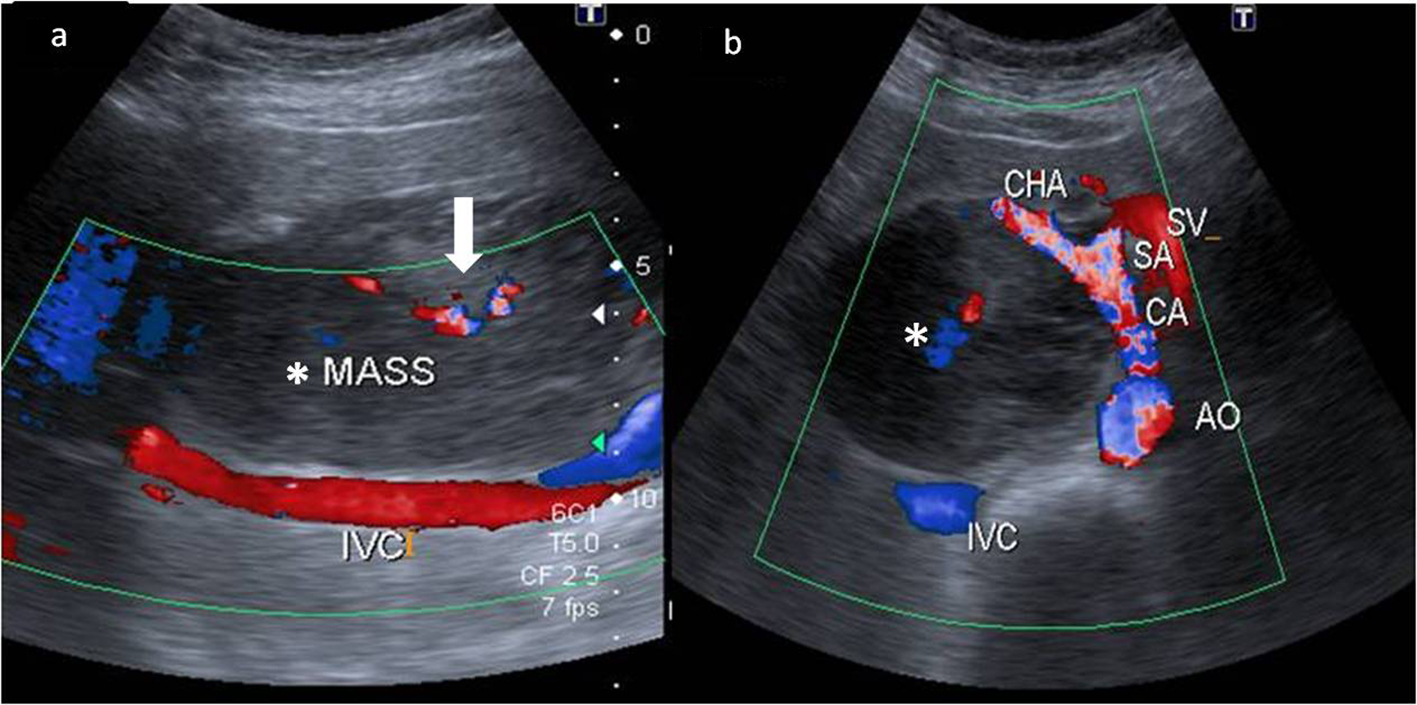
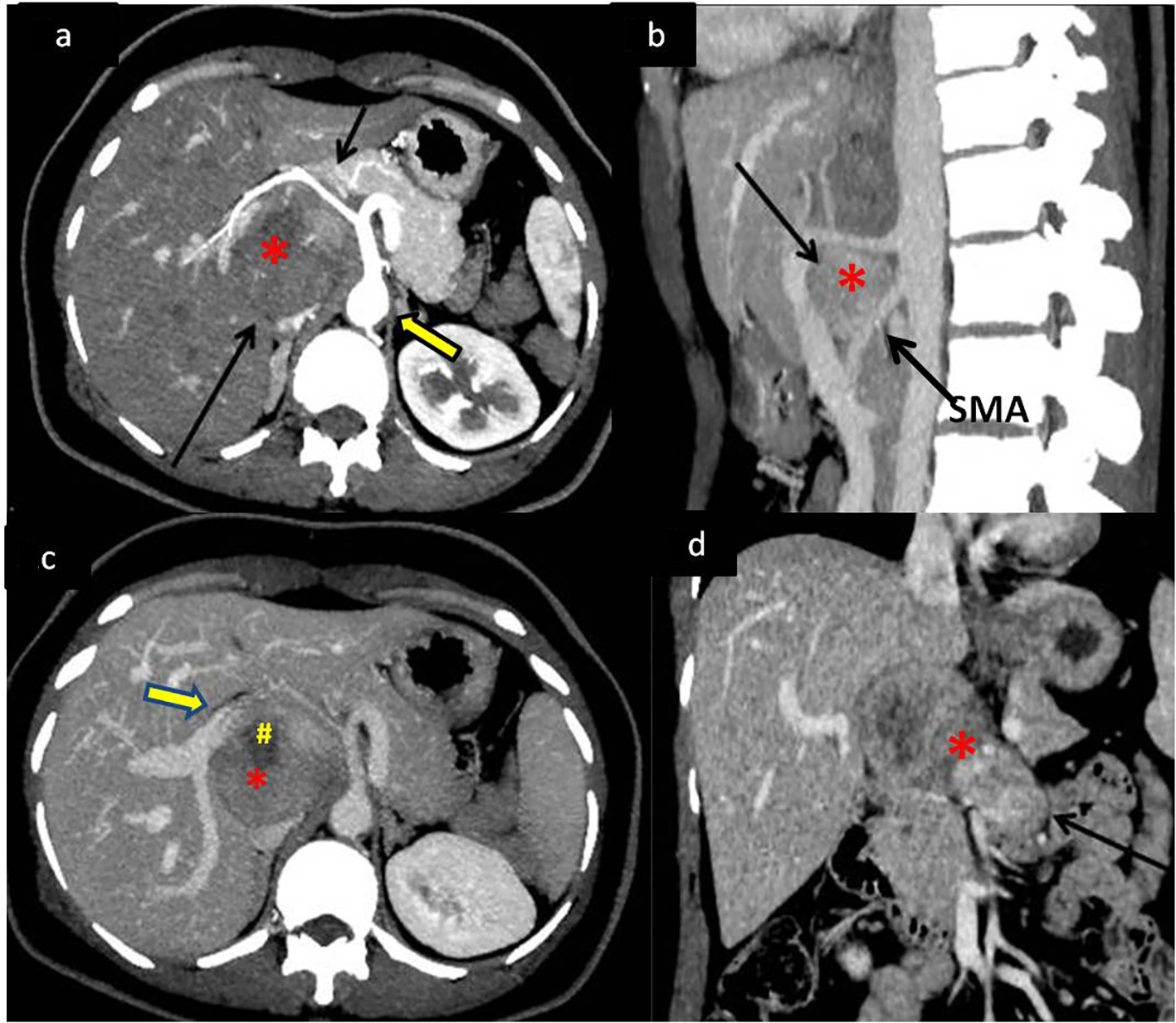
| Radiological findings | Large soft tissue enhancing mass with areas of necrosis, hemorrhage cystic spaces and rarely calcification [15] | Exophytic soft tissue mass projecting outside or inside the gastrointestinal lumen with ulceration and fistulous track formation , bowel dilation, ascites and omental caking [5, 16] |
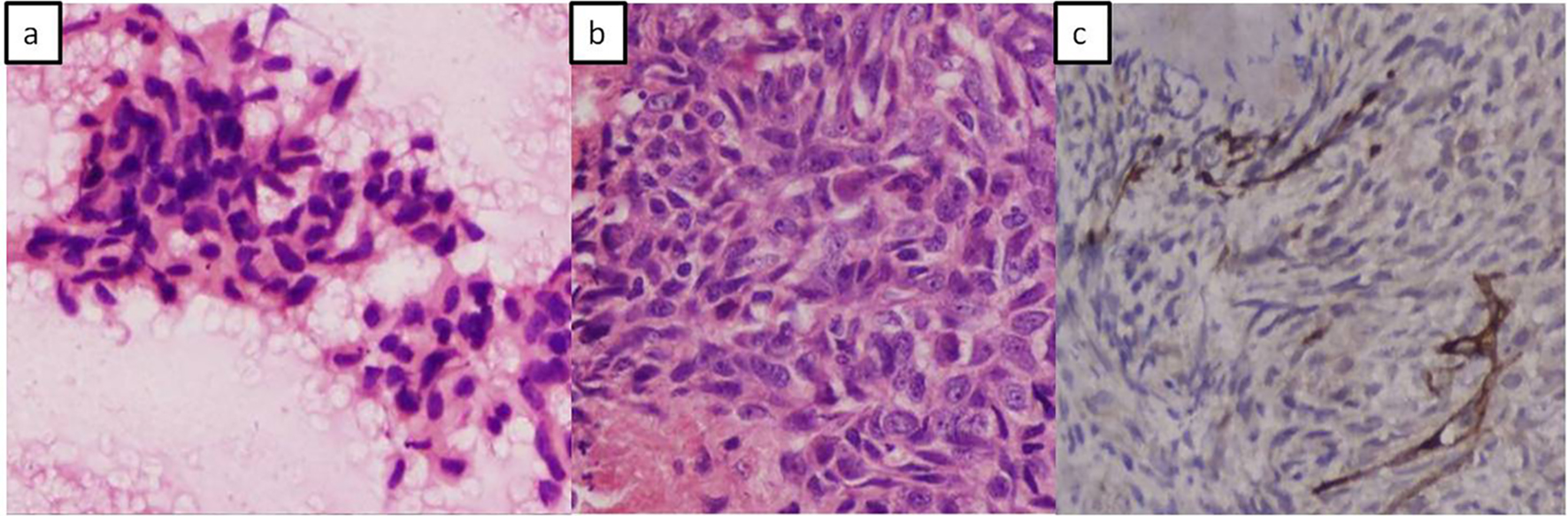
| Histopathology | Spindle cell type, epithelioid type [17] | Spindle (70%), epithelioid (20%), mixed (< 10%) type [7, 16] |
| Immunohistochemistry | Positive staining for CD117 for confirmation. Staining for other immunological markers is variable: BCL-2 (80%), CD34 (70%), smooth muscle actin (35%), S100 (10%), and desmin (5%) [17] | |
| Disease spread/metastasis | Direct spread into the peritoneum and retroperitoneum | Peritoneum, liver |
| General pathologic consensus for grading and prognosis | None devised so far | Standard consensus available based on tumor size and mitotic count [18] |
| Differential diagnosis on imaging [7] | Lymphoma
Sarcoma/mesenchymal tumor of the involved organ such as malignant fibrous histiocytoma, liposarcoma, leiomyosarcoma, fibrosarcoma | Adenocarcinomas of the bowel [5] |
| Management | Surgical resection/imatinib therapy [12] | Complete surgical resection for non-metastatic disease followed by imatinib as adjuvant therapy |
| Prognosis | Worse than GIST , usually more aggressive [13] | Long-term recurrence seen, only 10% free of disease at 10 years |