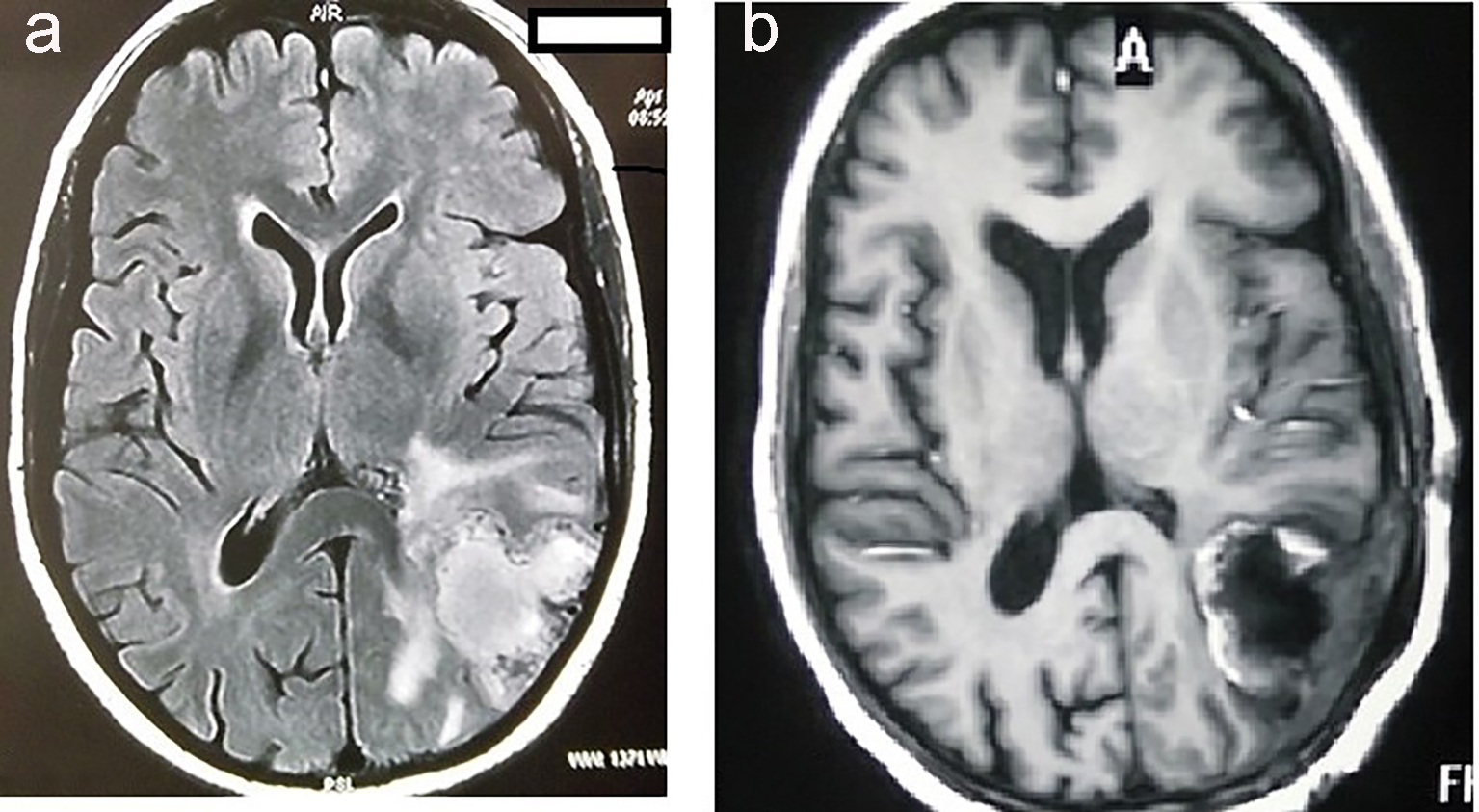
Figure 1. MRI of brain showing hyperintensity in the parieto-occipital lobe of brain (a). MRI of brain showing postoperative defect after complete excision of tumor (b).
| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website http://www.wjon.org |
Case Report
Volume 8, Number 2, April 2017, pages 53-57
Gliosarcoma in Young Adults: A Rare Variant of Glioblastoma
Figures
Table
| Patients | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Age | 35 years | 35 years | 16 years | 23 years |
| Sex | Male | Female | Male | Female |
| Site of tumor | Frontal lobe | Parieto-occipital lobe | Fronto-temporo-parietal region | Frontal lobe |
| Surgery | Complete macroscopic tumor removal | Gross total excision | Fronto-temporo-parietal craniotomy with cyst decompression and excision | Gross total excision |
| Radiotherapy | 60 Gy/30 fractions Over 6 weeks with concurrent temozolmide | 60 Gy/30 fractions Over 6 weeks with concurrent temozolmide | 60 Gy/30 fractions Over 6 weeks with concurrent temozolmide | 60 Gy/30 fractions Over 6 weeks with concurrent temozolmide |
| Chemotherapy | Six cycles with temozolomide | Six cycles with temozolomide | Six cycles with temozolomide | Six cycles with temozolomide |
| Follow-up (months) | Recurrence after 1.5 years, re-excision followed by six cycles chemotherapy with temozolomide. Now on follow-up for 9 months | 6 months | 4 months | 11 months |