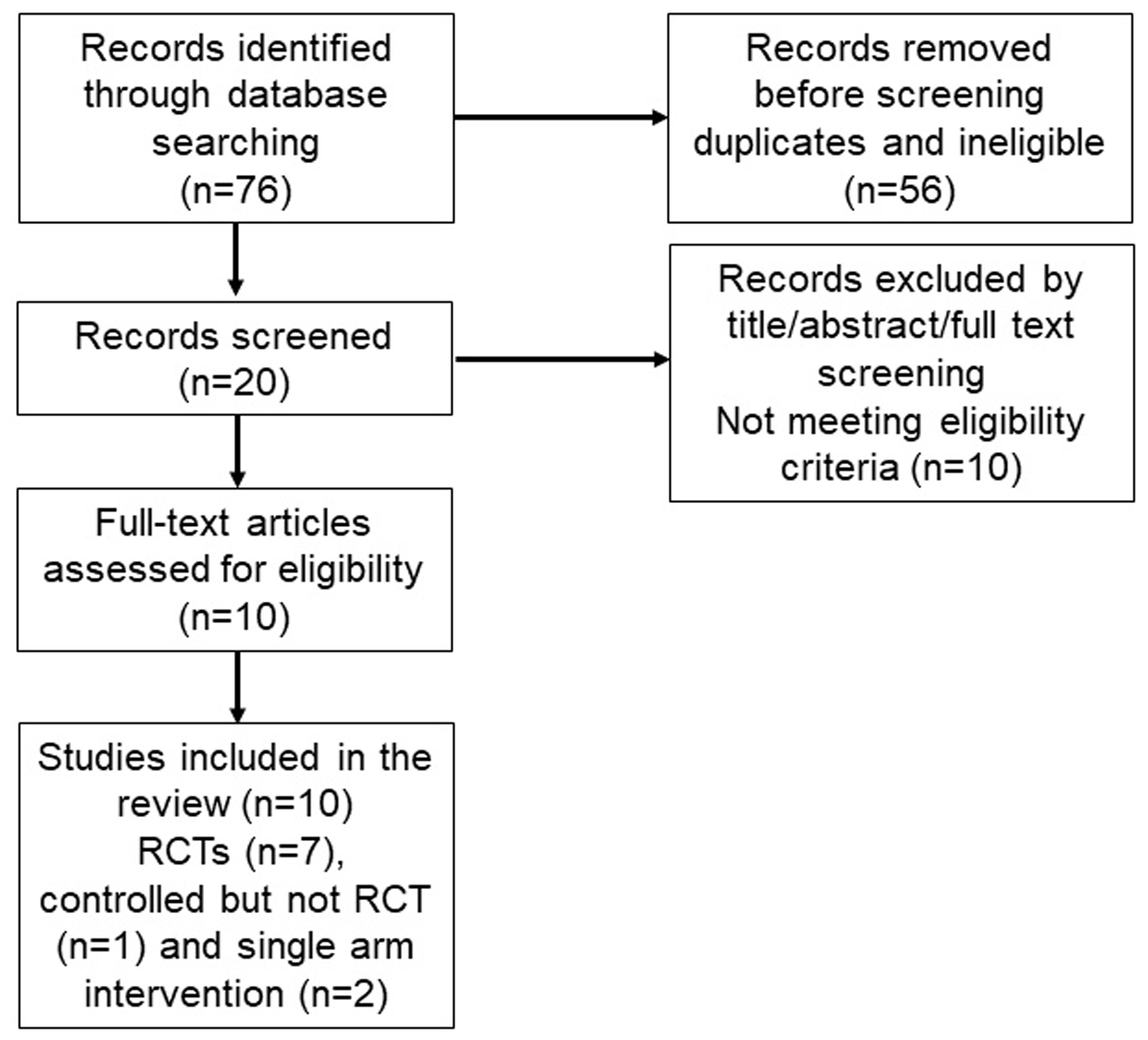
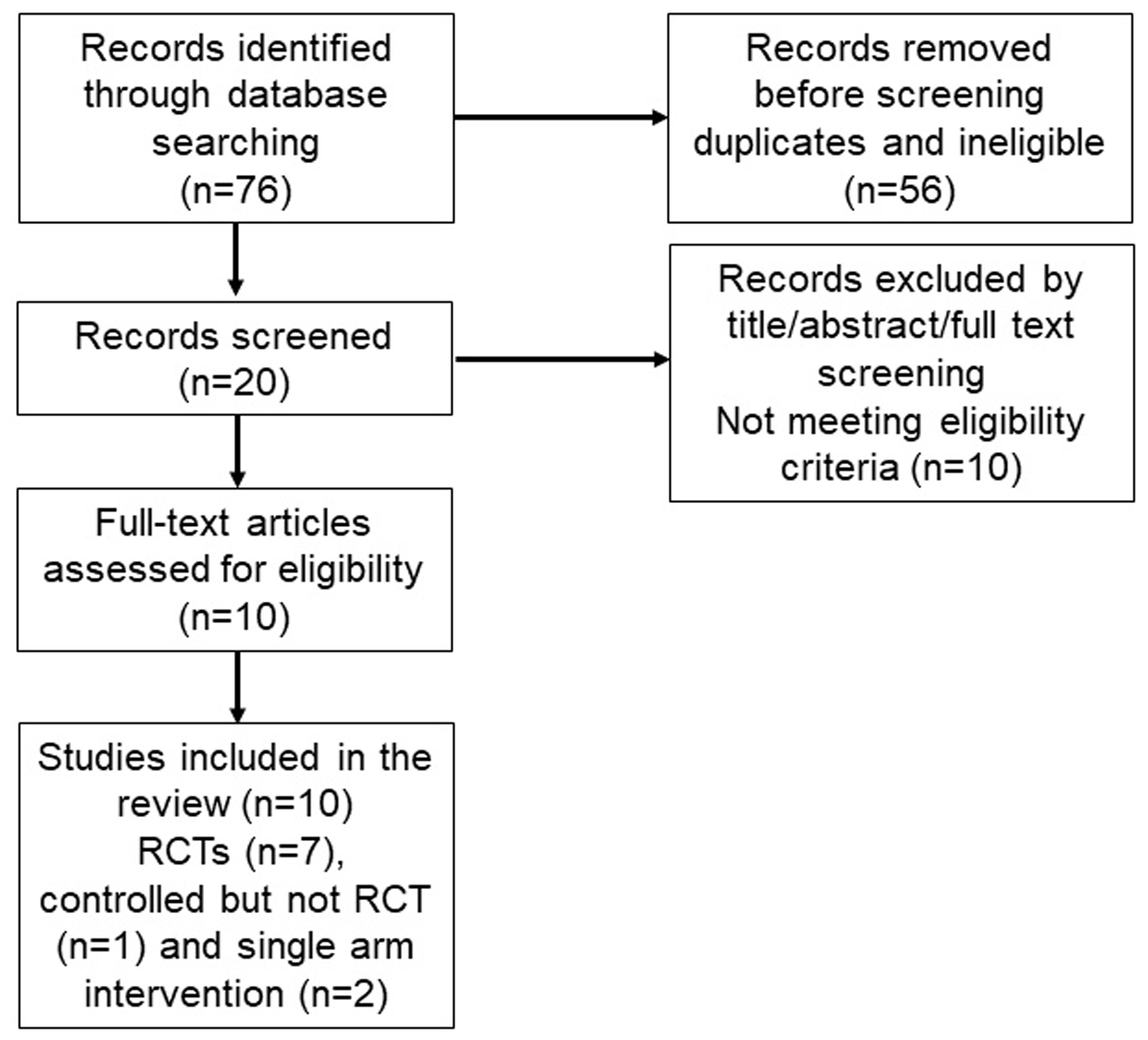
Figure 1. PRISMA flow diagram of literature search and studies selection.
| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Review
Volume 15, Number 3, June 2024, pages 337-347
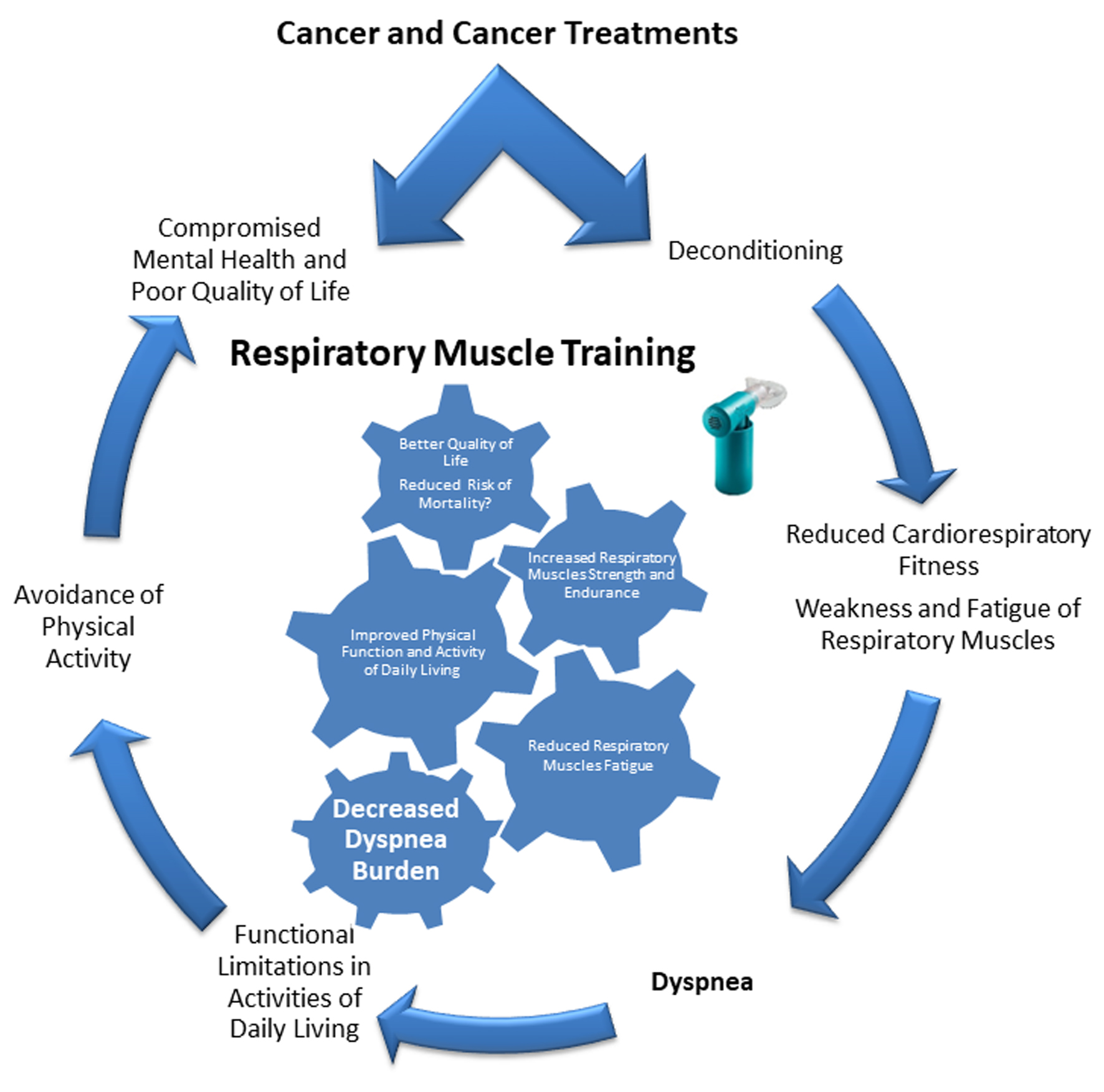
Potential Therapeutic Role of Respiratory Muscle Training in Dyspnea Management of Cancer Survivors: A Narrative Review
Figures
Table
| Study | Cancer patients | Intervention | Outcomes |
|---|---|---|---|
| Ray et al, 2017 [10] Single arm intervention | Breast (n = 5) and lung (n = 5) | Respiratory muscle training including both inspiratory and expiratory muscles (once a week supervised session + twice a week home-based). Three sets of 15 repetitions, three times a week for 4 weeks. | Reduction in dyspnea Baseline Dyspnea Index (+1.2 units) Transitional Dyspnea Index (+5.1 units) |
| Dahhak et al, 2022 [11] Randomized controlled trial | Breast (n = 19) | Twelve-week exercise training + inspiratory muscle training versus exercise training alone. | Reduction in dyspnea Transitional Dyspnea Index (+2.9) |
| Stefanelli et al, 2013 [12] Randomized controlled trial | Non-small cell lung cancer (n = 40) | Three weeks 5 days a week preoperative pulmonary rehabilitation combined with breathing exercises but not specifically respiratory muscle training versus usual care. | Reduced dyspnea Borg Dyspnea Scale (-1.1 units) |
| Molassiotis et al, 2015 [13] Randomized controlled trial | Stable lung cancer (n = 46) | Inspiratory muscle training, 30 min a day, 5 days a week for 12 weeks. | Reduction in dyspnea Modified Borg Dyspnea Scale (-0.8 units) |
| Sakai et al, 2023 [17] Controlled trial | Hospitalized stable lung cancer (n = 66) | Inspiratory muscle training + exercise therapy, 30 breaths twice a day at 30-40% of maximal inspiratory pressure + 20 - 40 min exercise therapy, 5 days a week for 2 weeks. | Reduction in dyspnea on exertion Modified Borg Dyspnea Scale (-1 units) |
| Palmer et al, 2019 [16] Single arm intervention | Head and neck cancer (n = 6) | Expiratory muscle training for 4 weeks | Reduction in dyspnea by 38% in Dyspnea Index (-2.3 units) |
| Ha et al, 2023 [57] Randomized controlled trial | Lung cancer (n = 22) | Virtual telemedicine-based inspiratory muscle training + walking intervention, inspiratory muscle training 10 - 15 min twice daily 5 days a week + walking four times a week for a total 12 weeks. Video conferences were every 2 weeks (six in total). | No significant difference in dyspnea versus control group (education only) |
| de Almeida et al, 2020 [58] Randomized controlled trial | Hospitalized hematopoietic stem cell transplantation (n = 31) | Physical rehabilitation (aerobic exercise) + inspiratory muscle training (40% of maximal inspiratory pressure, 10 - 20 min, 5 days/week). | Trend towards lower dyspnea prevalence in the intervention group but did reach statistically significant difference versus control group (aerobic exercise only) |
| Bargi et al, 2016 [14] Randomized controlled trial | Allogenic hematopoietic stem cell transplantation (n = 38) | Inspiratory muscle training (40% of maximal inspiratory pressure, 30 min/day, 7 days/week for 6 weeks) vs. sham (5% of maximal inspiratory pressure, 30 min/day, 7 days/week for 6 weeks). | Reduction in dyspnea Modified Borg Dyspnea Scale (-0.11 units) |
| Bayram et al, 2023 [15] Randomized controlled trial | Hematopoietic stem cell transplantation (n = 30) | Pulmonary rehabilitation (resistance training) + inspiratory muscle training (30% of maximal inspiratory pressure, 8 - 10 diaphragmatic breathings, two session/day, 5 days/week) vs. aerobic exercise 10 - 30 min for upper body 5 days/week). | Reduction in dyspnea Modified Borg Dyspnea Scale (-0.9 units) |