| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website http://www.wjon.org |
Case Report
Volume 9, Number 4, August 2018, pages 110-114
Adenocarcinoma of Lung and Bronchial Carcinoid Presenting as Double Synchronous Primary Lung Cancer: A Case Report and Review of Literature
Lakshmi Saladia, d, Sai Mounica Maddub, Masooma Niazic, Ajsza Matelaa
aDivision of Pulmonary and Critical Care Medicine, Department of Medicine, Bronx Care Health System, Bronx, NY 10457, USA
bDepartment of Medicine, Bronx Care Health System, Bronx, NY 10457, USA
cDepartment of Pathology, Bronx Care Health System, Bronx, NY 10457, USA
dCorresponding Author: Lakshmi Saladi, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Bronx Care Health System, Bronx, NY 10457, USA
Manuscript submitted June 13, 2018, accepted June 26, 2018
Short title: Double Synchronous Primary Lung Cancer
doi: https://doi.org/10.14740/wjon1129w
| Abstract | ▴Top |
Recent advances in imaging techniques led to an increase in the incidence of synchronous and metachronous primary lung cancers due to early detection. Management of these patients is challenging and prognosis depends on the stage of the tumor at initial diagnosis and histological type. A 68-year-old African American male patient with medical history of hypertension and diabetes mellitus presented to our emergency department with right sided chest pain, worsening dyspnea and dry cough of 2-week duration. He also reported significant weight loss and was a smoker with 25 pack-years smoking history. Chest radiology showed a large right pleural effusion. Subsequent thoracentesis and fluid analysis revealed a lymphocytic exudate. Patient underwent bronchoscopy with findings of an endobronchial lesion in the left lower bronchus. Microscopic analysis of the biopsy specimen showed a well differentiated carcinoid. It was decided to proceed with VATS and pleural biopsy as part of workup for unexplained exudative pleural effusion. Multiple pleural nodules were detected during the procedure and biopsy of these nodules revealed adenocarcinoma of lung. He was evaluated by Oncology and underwent palliative chemotherapy. The association of carcinoid with adenocarcinoma of lung was infrequently reported in the past. This case also highlights the importance of additional diagnostic workup for primary when the diagnosed malignancy does not explain the clinical presentation.
Keywords: Pleural effusion; Smoking; Bronchoscopy; Dyspnea; Neuroendocrine tumor
| Introduction | ▴Top |
Despite advances in technology, the incidence of lung cancer is increasing and remains the most common cause of cancer-related deaths. Multiple primary lung cancers are rare and can be synchronous or metachronous. When different primary lung cancers are simultaneously detected in a patient, they are referred to as synchronous primary lung cancers. Metachronous cancers are tumors that occur at different times in the same patient. If the tumors are histologically identical, a tumor-free period of at least 2 years is required for diagnosis. Diagnosis of these cancers remains a challenge as multiple lesions on imaging can be mistaken for a metastatic tumor. The distinction between the two has great therapeutic and prognostic implications. We report a case of a 68-year-old man who presented to our hospital with a massive right pleural effusion. He was diagnosed with synchronous carcinoid and adenocarcinoma of the lung with pleural metastasis. We also present a detailed discussion on literature published in the past and optimal management of these patients.
| Case Report | ▴Top |
A 68-year-old man presented to the emergency room with right sided chest pain, worsening dyspnea and dry cough of 2-week duration. He also reported weight loss of 40 pounds in 2 months without fever or night sweats. His medical history was significant for hypertension and diabetes mellitus. He had a left below knee amputation in 2010. He had no family history of lung disease or cancers. He was a smoker with 25 pack-years smoking history and admitted using marijuana occasionally. He was from Jamaica and immigrated to the United States in 1982.
Physical examination revealed a thin, cachectic man with digital clubbing, a systolic murmur along left sternal border and decreased air entry on the right side. There was no palpable lymphadenopathy. He had a chest X-ray on arrival which showed massive right pleural effusion with compression of the heart and had emergent chest tube placement (Fig. 1). Pleural fluid was serosanguinous and analysis was consistent with a lymphocytic exudate, cultures remained negative and fluid cytology was negative for malignant cells. CT scan of the chest revealed a loculated right pleural effusion and mediastinal adenopathy (Fig. 2). He underwent a repeat thoracentesis and fluid cytology was positive for atypical cells. Laboratory parameters are shown in Table 1.
 Click for large image | Figure 1. Chest X-ray showing complete right hemithorax opacification with mediastinal shift to the left. |
 Click for large image | Figure 2. (a) Coronal view CT chest showing massive right pleural effusion with atelectasis of right lung and mediastinal shift to the left. (b) Sagittal view of CT chest showing massive right pleural effusion with atelectasis of right lung and mediastinal shift to the left. |
 Click to view | Table 1. Laboratory Parameters |
Fiberoptic bronchoscopy and EBUS guided transbronchial needle aspiration of subcarinal and right lower paratracheal lymph nodes were performed. There was an endobronchial lesion in the left lower bronchus, pathology revealed neuroendocrine tumor consistent with well differentiated carcinoid (Fig. 3). Immunohistochemistry was positive for TTF-1, synaptophysin, chromogranin, CD56 and negative for CK-7, CD20 and LCA (Fig. 4). Mediastinal node sampling was negative for malignancy. Patient underwent right sided VATS for pleural effusion of unknown etiology and was found to have multiple pleural nodules. The biopsy of these nodules was consistent with lung adenocarcinoma. Immunohistochemistry was positive for CK-7, TTF-1, CDX-2 and negative for synaptophysin, chromogranin, napsin-A, CK-20 (Fig. 5). The tumor was negative for EGFR, KRAS mutations, ALK rearrangement and PD-L1 expression. He had a Pleurex catheter placed for long-term drainage of effusion.
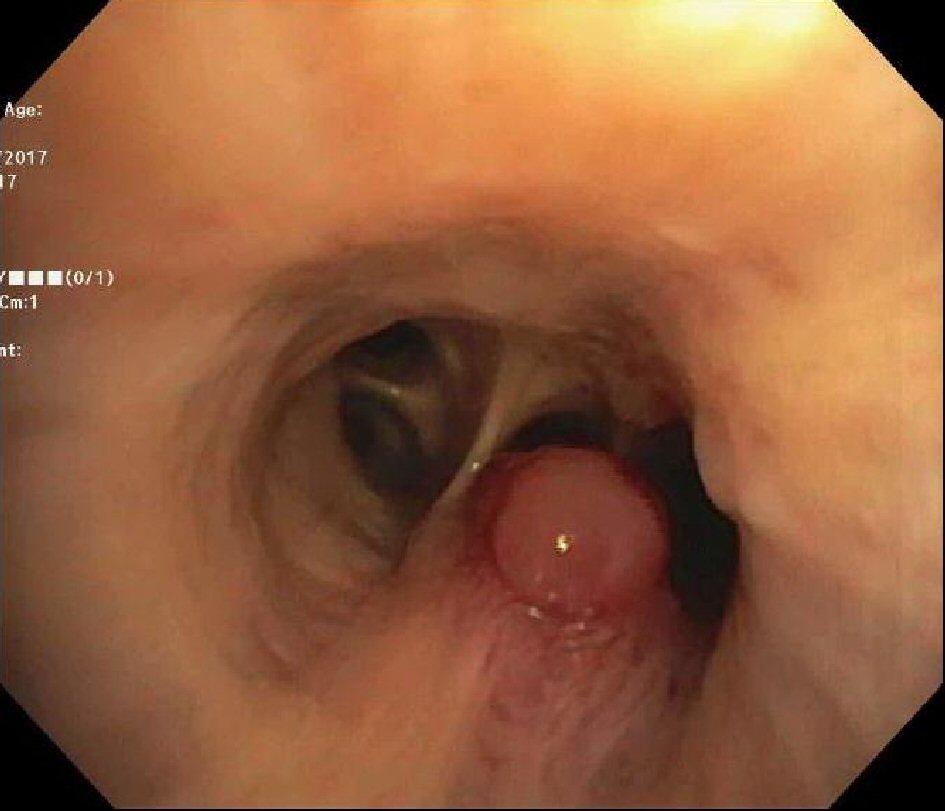 Click for large image | Figure 3. Fiberoptic bronchoscopy revealed an endobronchial lesion in left lower bronchus. |
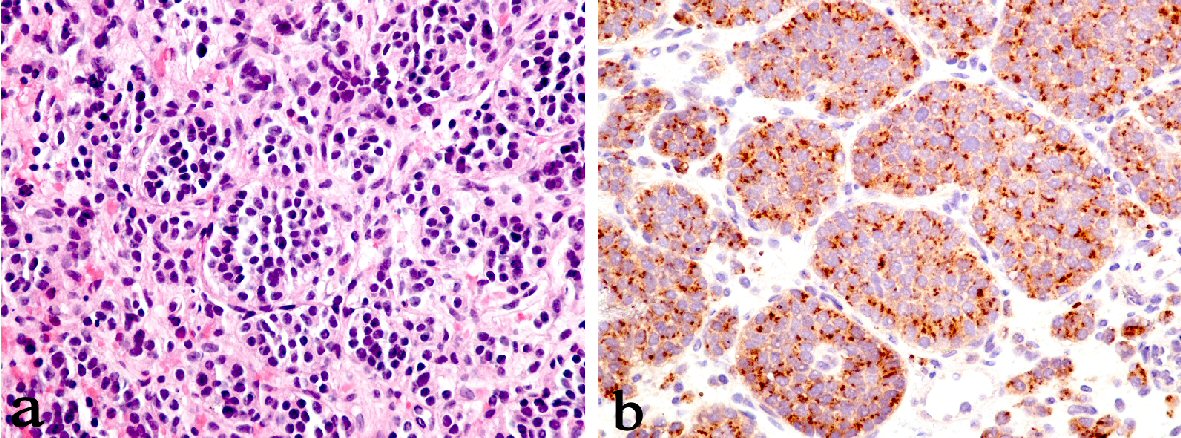 Click for large image | Figure 4. (a) Endobronchial biopsy: carcinoid tumor, high power of organoid pattern with uniform nuclei and no mitosis or necrosis (H&E, magnification × 400). (b) Carcinoid tumor: the tumor cells are immunoreactive to neuroendocrine marker chromogranin (magnification × 400). |
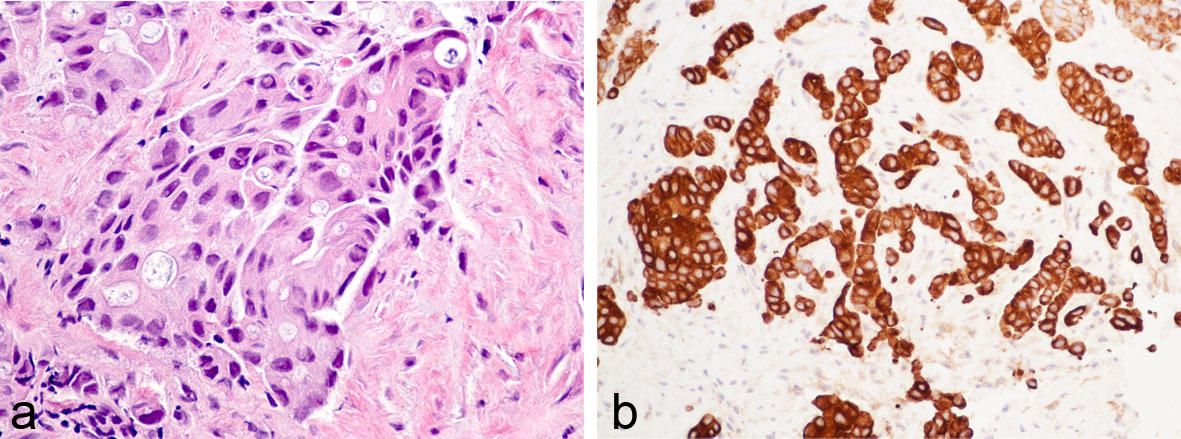 Click for large image | Figure 5. (a) Pleural mass biopsy on high magnification showing acinar pattern of adenocarcinoma composed of glands lined by malignant cells. Some cells show cytoplasmic vacuoles (H&E, magnification × 400). (b) Pleural mass biopsy: the malignant cells are strongly positive for immunomarker cytokeratin -7, which supports the diagnosis of lung primary (magnification × 400). |
There was no evidence of metastasis to brain and bone. He was evaluated by Oncology and discharged to a rehabilitation facility with a plan for palliative chemotherapy considering metastasis to pleura.
| Discussion | ▴Top |
The first case of multiple primary lung malignancies was reported in 1924 by Beyreuther in post mortem studies, which was a well differentiated squamous cell carcinoma in right lung and adenocarcinoma in left lung [1]. Since then, there have been many case reports and studies describing multiple primary lung cancers with association of squamous cell with squamous cell cancer being the most common followed by squamous cell and small cell carcinoma [2]. The incidence of these cancers, as reported in previous studies, is variable ranging from less than 1% to as high as 16%. Synchronous lung cancers are significantly rarer than metachronous cancers with an average incidence of 0.5% of all lung cancers [3].
Warren and Gates published the original criteria for multiple lung cancers in 1932 [4]. Martini and Melamed in 1975 suggested that to diagnose multiple synchronous primary lung tumors, each tumor should be physically distinct from the other and should be malignant with a different histology. If histology is same, tumor should be located in a different segment, lobe or lung; with absence of carcinoma in common lymphatics and exclusion of extrapulmonary metastasis [5]. In 1995, Antakli et al added DNA ploidy to the diagnostic criteria of tumors with identical histology [6]. The criteria were further modified by the American College of Chest Physicians in 2007 and the update suggests a possibility of metastasis rather than a second primary lung cancer in patients with either a synchronous or a metachronous presentation with an interval of less than 4 years between tumors. The outcomes are variable and generally poor after resection in such patients [7].
Smoking related carcinogenic insults, leading to cellular atypia and allele-specific imbalance in different areas of bronchial mucosa, has been implicated as the cause of multifocality of these lung tumors in several studies [8, 9]. The association of lung adenocarcinoma and bronchial carcinoid is extremely rare and one such report was published in 1966 by Roberts and Cumming [10]. In 1980, Ranchod and Levine published a series of 35 patients with spindle cell carcinoid tumor of which one patient had evidence of adenosquamous carcinoma in the resected specimen [11].
Nagamatsu et al reported a case of cancer-in-cancer and the resected specimen showed a carcinoid component localized within the central fibrous scar of the dominant adenocarcinoma component [12]. A case of five synchronous and metachronous lung cancers in a single patient that developed in a span of 7 years was reported in 2004. The synchronous malignancies were poorly differentiated squamous cell carcinoma, moderately differentiated adenocarcinoma and a small typical carcinoid [13]. A case of triple synchronous lung cancer with bronchial carcinoid, small cell carcinoma and adenocarcinoma of the lung was reported in 1986 by Jung-Legg et al. This patient also had a rectal carcinoid [14]. Yano and colleagues reported another case of bronchial carcinoid and lung adenocarcinoma in 2002 [15].
The optimal management of patients with multiple primary lung tumors is controversial. If the clinical stage of the tumor and functional status of the patient permit, surgery is the treatment of choice. The two tumors should be staged separately and extensive mediastinal staging and imaging to rule out metastasis is required prior to surgical resection. Stereotactic body radiation therapy (SBRT) is a novel radiation therapy which has been used in lung cancer management. The 5-year survival in retrospective studies in patients who underwent SBRT was between 51% and 70% [16]. Chang et al reported a 2-year survival rate of 61.5% and 4-year survival rate of 39% with stereotactic ablative radiotherapy (SABR) in early stage multiple synchronous lung cancers with contraindications to surgical resection [17]. An aggressive surgical approach in patients with synchronous lung cancers was shown to have a similar survival benefit when compared to single lung cancer by Finley et al in 2010 [18].
The prognosis of patients with synchronous or early metachronous (< 2 years) was shown to be worse when compared with late metachronous (> 2 years) lung cancers [19]. In a study of 346 post-surgical patients with stage I non-small cell lung cancer, Pairolero et al reported a survival of 51% in patients with a second primary lung tumor at the end of 2 years where as the survival for patients with local recurrence and distant metastasis was 23% and 8% respectively [20]. In 1989, van Bodegom et al demonstrated that patients with multiple primary cancers have a better survival than advanced tumors [21]. Since the year 2000, there were more than 20 reported cases and 20 original studies that mainly analyzed the long-term prognosis of patients with synchronous primary lung cancers. A systemic review and meta-analysis of 1,796 patients with multiple primary lung cancers in 22 studies confirmed a better survival in these patients when compared to intrapulmonary metastasis [22].
Our patient had a rare association of bronchial carcinoid with metastatic adenocarcinoma of lung. As reported in previous studies, smoking could be a contributing factor for the development of synchronous lung cancers in our patient [23]. Although bronchoscopy revealed an endobronchial lesion which later revealed a carcinoid tumor, it was decided to proceed with VATS for further evaluation of his pleural effusion of unknown etiology. It was unfortunate that our patient had stage IV adenocarcinoma with pleural metastasis at the time of presentation. Hence, the only treatment that could be offered was palliative chemotherapy.
Conclusions
The frequency of synchronous multiple primary lung cancers has been increasing in the recent years because of the development of early detection techniques and advances in cancer therapy, thus improving patient survival. Nevertheless, the combination of adenocarcinoma with bronchial carcinoid has been described infrequently in the past. A high clinical suspicion for a second malignancy is essential in cases where initial diagnostic workup does not explain underlying clinical presentation. Early diagnosis when tumor is resectable can improve survival in patients with multiple primary lung tumors.
Disclosure
None of the authors has a financial relationship with a commercial entity that has an interest in the subject of the manuscript.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Abbreviations
ALK: anaplastic lymphoma kinase; CK-7: cytokeratin-7; CK-20: cytokeratin-20; CT: computed tomography; EBUS: endobronchial ultrasound; EGFR: epidermal growth factor receptor; LCA: leukocyte common antigen; PD-L1: programmed death ligand 1; TTF-1: thyroid transcription factor 1; VATS: video assisted thoracoscopic surgery; X-ray: roentgenogram
| References | ▴Top |
- Beyreuther H. Multipicate von carcinomen bei einem fall von sog. Schenecberger Lungenkrebs mit tuberkulose. Virchows Arch. 1924;250:230-243.
doi - Rohwedder JJ, Weatherbee L. Multiple primary bronchogenic carcinoma with a review of the literature. Am Rev Respir Dis. 1974;109(4):435-445.
pubmed - Ferguson MK. Synchronous primary lung cancers. Chest. 1993;103(4 Suppl):398S-400S.
doi pubmed - Warren S, Gates O. Multiple primary malignant tumors: a survey of the literature and a statistical study. Am J Cancer. 1932;16:1358-1414.
- Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg. 1975;70(4):606-612.
pubmed - Antakli T, Schaefer RF, Rutherford JE, Read RC. Second primary lung cancer. Ann Thorac Surg. 1995;59(4):863-866; discussion 867.
doi - Shen KR, Meyers BF, Larner JM, et al. American College of Chest Physicians, Special treatment issues in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132:S290-305.
- Auerbach O, Stout AP, Hammond EC, Garfinkel L. Changes in bronchial epithelium in relation to cigarette smoking and in relation to lung cancer. N Engl J Med. 1961;265:253-267.
doi pubmed - Sikkink SK, Liloglou T, Maloney P, Gosney JR, Field JK. In-depth analysis of molecular alterations within normal and tumour tissue from an entire bronchial tree. Int J Oncol. 2003;22(3):589-595.
pubmed - Roberts GH, Cumming RL. A case report of two primary tumours: bronchial carcinoid and adenocarcinoma in the same lung. Br J Dis Chest. 1966;60(3):160-163.
doi - Ranchod M, Levine GD. Spindle-cell carcinoid tumors of the lung: a clinicopathologic study of 35 cases. Am J Surg Pathol. 1980;4(4):315-331.
doi pubmed - Nagamatsu Y, Iwasaki Y, Omura H, Kumazoe H, Hyashida R, Shirouzu K. A case of resected synchronous multiple primary lung cancer comprising adenocarcinoma and carcinoid (cancer-in-cancer). Gen Thorac Cardiovasc Surg. 2012;60(8):518-521.
doi pubmed - Flynn MJ, Rassl D, El Shahira A, Higgins B, Barnard S. Metachronous and synchronous lung tumors: five malignant lung pathologies in 1 patient during 7 years. Ann Thorac Surg. 2004;78(6):2154-2155.
doi - Jung-Legg Y, McGowan SE, Sweeney KG, Zitzman JL, Pugatch RD. Synchronous triple malignant tumors of the lung. A case report of bronchial carcinoid, small cell carcinoma, and adenocarcinoma of the right lung. Am J Clin Pathol. 1986;85(1):96-101.
doi pubmed - Yano K, Yokoi K, Matsuguma H, Anraku M, Kondo T, Kamiyama Y, Mori K, et al. [Synchronous tumors consisted of bronchial carcinoid and adenocarcinoma of the lung]. Kyobu Geka. 2002;55(6):457-460.
pubmed - Onishi H, Shirato H, Nagata Y, Hiraoka M, Fujino M, Gomi K, Karasawa K, et al. Stereotactic body radiotherapy (SBRT) for operable stage I non-small-cell lung cancer: can SBRT be comparable to surgery? Int J Radiat Oncol Biol Phys. 2011;81(5):1352-1358.
doi pubmed - Chang JY, Liu YH, Zhu Z, Welsh JW, Gomez DR, Komaki R, Roth JA, et al. Stereotactic ablative radiotherapy: a potentially curable approach to early stage multiple primary lung cancer. Cancer. 2013;119(18):3402-3410.
doi pubmed - Finley DJ, Yoshizawa A, Travis W, Zhou Q, Seshan VE, Bains MS, Flores RM, et al. Predictors of outcomes after surgical treatment of synchronous primary lung cancers. J Thorac Oncol. 2010;5(2):197-205.
doi pubmed - Rosengart TK, Martini N, Ghosn P, Burt M. Multiple primary lung carcinomas: prognosis and treatment. Ann Thorac Surg. 1991;52(4):773-778; discussion 778-779.
doi - Pairolero PC, Williams DE, Bergstralh EJ, Piehler JM, Bernatz PE, Payne WS. Postsurgical stage I bronchogenic carcinoma: morbid implications of recurrent disease. Ann Thorac Surg. 1984;38(4):331-338.
doi - van Bodegom PC, Wagenaar SS, Corrin B, Baak JP, Berkel J, Vanderschueren RG. Second primary lung cancer: importance of long term follow up. Thorax. 1989;44(10):788-793.
doi pubmed - Jiang L, He J, Shi X, Shen J, Liang W, Yang C, He J. Prognosis of synchronous and metachronous multiple primary lung cancers: systematic review and meta-analysis. Lung Cancer. 2015;87(3):303-310.
doi pubmed - Xue X, Xue Q, Wang N, Zhang L, Guo L, Li X, Sun J, et al. Early clinical diagnosis of synchronous multiple primary lung cancer. Oncol Lett. 2012;3(1):234-237.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


