| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Case Report
Volume 14, Number 6, December 2023, pages 584-588
Borderline Phyllodes Tumor in a Child
Esperanza Millan-Arreolaa , Diego Alberto Lozano-Jaramilloa, b, c
, Aida Tello De Meneses-Salazara, Oscar Omar Esquer-Cotaa, Luz Adriana Lavara-Mirandaa, Miguel Alfonso Valenzuela-Espinozaa
aCentro Oncologico Pediatrico de Baja California, Tijuana, Mexico
bCentro de Investigacion Valle Bibb Fundacion, Tijuana, Mexico
cCorresponding Author: Diego Alberto Lozano-Jaramillo, Centro de Investigacion Valle Bibb Fundacion, Centro Oncologico Pediatrico de Baja California, Etapa, 22450 Tijuana, BC, Mexico
Manuscript submitted August 23, 2023, accepted September 12, 2023, published online October 21, 2023
Short title: Borderline Phyllodes Tumor in a Child
doi: https://doi.org/10.14740/wjon1716
| Abstract | ▴Top |
Phyllodes tumor (PT) is considered a rare fibroepithelial tumor. Very few series have been reported in children and adolescents. Based on histopathological features, it can be classified as benign, borderline, or malignant, with the latter having a more aggressive clinical behavior. We report the case of a 10-year-old female who began with an asymptomatic mobile right breast mass. An initial fine needle biopsy (FNB) concluded fibroadenoma (FA). Months later, the mass kept growing, with the appearance of pain and nipple discharge. Benign PT was demonstrated in a new biopsy. A total mastectomy was performed. The post-surgical histopathological examination was compatible with a borderline PT. The patient is now symptom-free and with no signs of relapse. Not all breast masses in the pediatric or adolescent age bracket are FA. Attention is warranted when the clinical behavior does not follow the usual outline. PT has to be considered as a possible diagnosis and treated accordingly.
Keywords: Fibroadenoma; Fine needle biopsy: Pediatric breast masses; Phyllodes tumor
| Introduction | ▴Top |
Pediatric breast masses (PBMs) are not rare in children and adolescents, with an estimated incidence of 3.2% [1]. The most common findings in surgically removed breast masses in this age bracket are fibroadenomas (FAs). Breast carcinoma corresponds to only 0.02% of the cases [2]. Phyllodes tumor (PT) is a rare fibroepithelial tumor accounting for 0.3-0.5% of all breast tumors in females [3]. It is regarded as a rare disease in children and adolescents since very few large series of PT exist [4]. The World Health Organization (WHO) classifies them histologically as benign, borderline, or malignant, with the latter having a more aggressive clinical behavior [5]. Treatment typically involves breast-conserving surgery or mastectomy, depending on the histological grade and clinical features [6, 7]. Only a few reports of malignant or borderline PT in children and in the adolescents and young adults (AYA) age bracket have been reported [8-10]. We present the case of a 10-year-old female with a rapidly growing right breast mass due to a borderline PT who was treated effectively with a total mastectomy.
| Case Report | ▴Top |
Investigations
A 10-year-old female previously healthy and with no medical history initiated a year prior to final diagnosis with a partially mobile right breast mass of approximately 1 × 1.5 cm. Three months later, pain and edema began. A month later, collateral veins appeared, the pain intensified, and spontaneous drainage of serous material through the nipple was noted. Laboratory exams were issued with no anomalies, with cancer antigen 125 at 11.90 U/mL. She was given antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) with no improvement. Fine needle biopsy (FNB) concluded FA; no further follow-up or treatment was given. After 5 months, the mass increased exponentially until it occupied the whole breast with a diameter of 20 cm, as shown in Figure 1. Upper right extremity mobility was limited due to mass size. Pain and discharge on the nipple became persistent.
 Click for large image | Figure 1. Large right breast mass with multiple collateral veins and ulceration of the nipple. Note the normal left breast. |
Diagnosis
A new FNB was performed and analyzed by two different pathologists. Both reported neoplastic proliferation due to stromal hypercellularity with an exaggerated intracanalicular pattern with leaf-like fronds protruding into dilated spaces, concluding benign PT. A referral to our pediatric cancer center was made.
Treatment
Even though the biopsy yielded a benign PT, a multidisciplinary consensus was made that a total mastectomy was to be performed, due to the size of the mass and the burden of the symptoms. Surgery was performed complications-free, and the patient was discharged after a day of observation. The macroscopic examination of the specimen reported a weight of 1,500 g with dimensions of 23 × 20 × 10 cm (Fig. 2). Microscopically borders were tumor-free and histologically compatible with a borderline PT. Immunohistochemical stains yielded negativity in the malignant cell nucleus for human epidermal growth factor receptor (HER)2 neu and positivity for estrogen and progestogen in 80% and 70%, respectively. The proliferation marker Ki-67 resulted in a low proliferation index (Fig. 3).
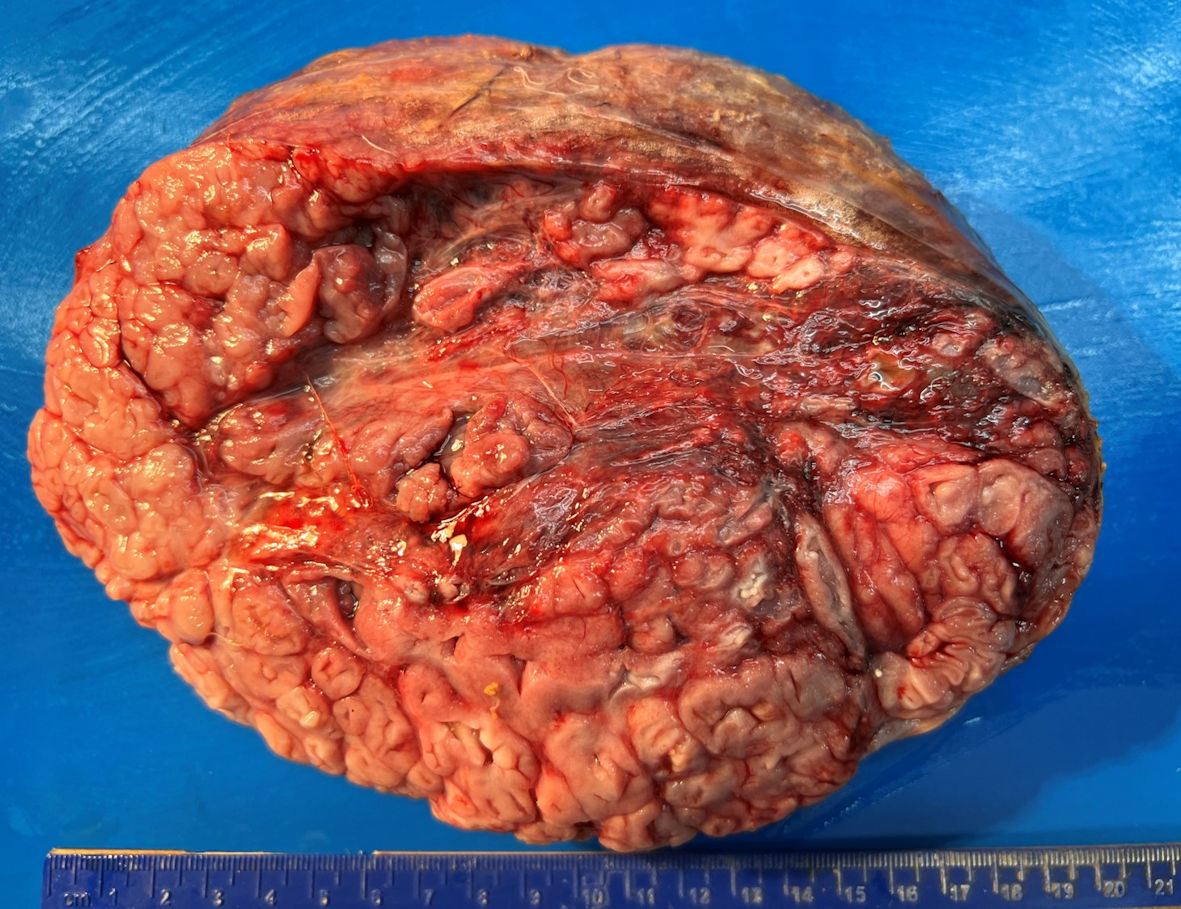 Click for large image | Figure 2. Macroscopic examination of mastectomy shows multinodular mass with pseudocystical and mucoid aspect and 20 cm of diameter. |
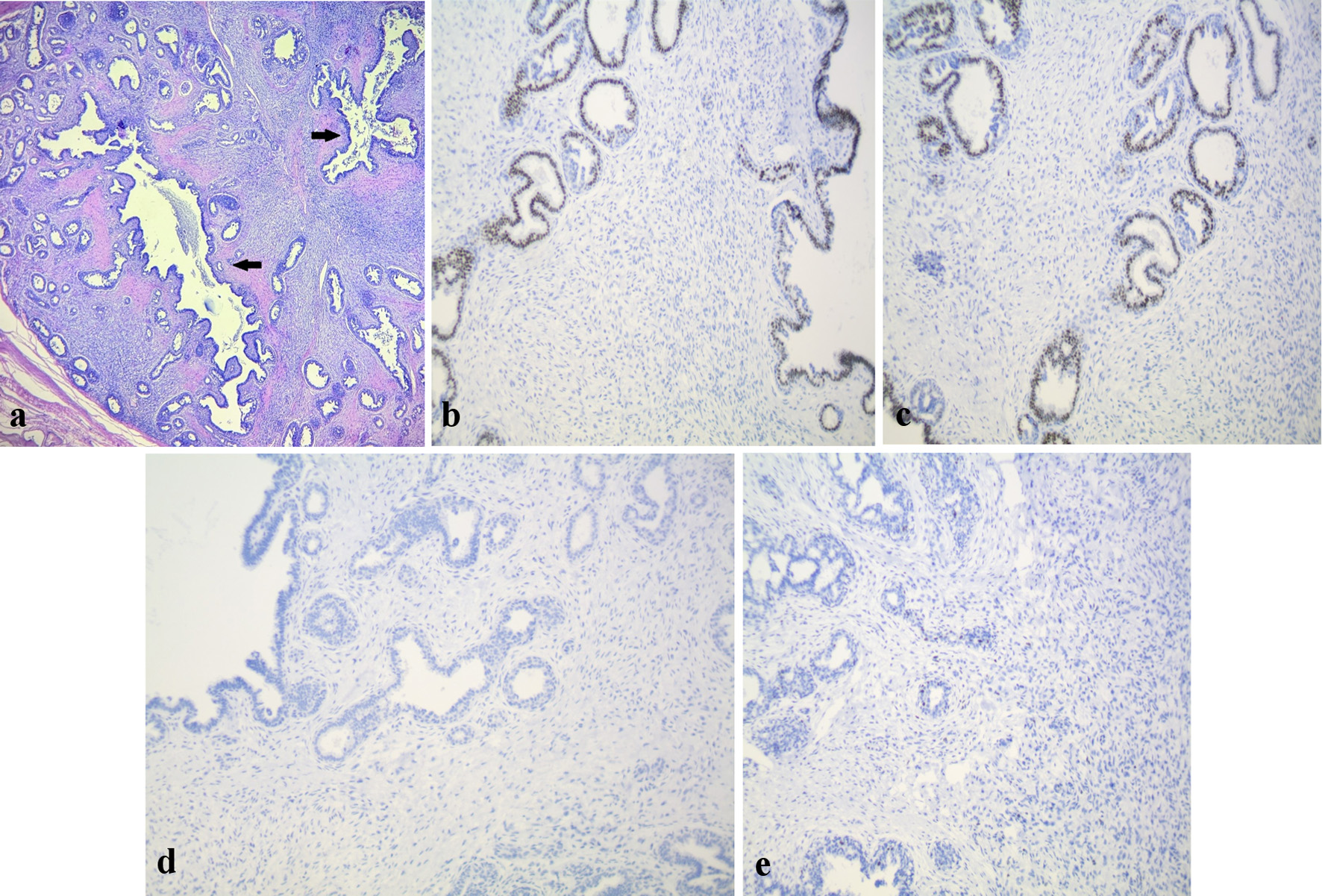 Click for large image | Figure 3. (a) H&E stain (× 10) shows stroma with nodular enlargement and a leaf-like pattern (arrows). (b) IHC estrogen receptor (× 20) stain shows positive immunoreactivity in 80% of malignant cells. (c) IHC progesterone receptor stain (× 20) shows positive immunoreactivity in 70% of malignant cells. (d) HER2 stain (× 20) shows no immunoreactivity. (e) Ki-67 stain (× 10) shows less than 2% of nuclear immunoreactivity on epithelial cells. IHC: immunohistochemistry; H&E: hematoxylin and eosin; HER: human epidermal growth factor receptor. |
Follow-up and outcomes
During the 10-month follow-up after the surgical intervention, the patient presented mild edema and pain that eventually disappeared. During her last visit she reported being symptom-free and with a better quality of life.
| Discussion | ▴Top |
PT is a rare fibroepithelial neoplasm that resembles FA in its clinical and histopathological presentation. Clinically, PT presents as a large mass that grows rapidly, typically larger than 6 cm. This makes them difficult to differentiate from giant or juvenile FA [11]. Initially, our patient had the clinical evolution of an FA with a small to mid-size breast mass. This mass grew exponentially, impacting her quality of life, which promoted reassessing the diagnosis. Although it can be thought in this specific age bracket that a larger mass can raise the question of malignancy, McLaughlin et al [12] found no association between size and final diagnosis for malignancy. A core needle biopsy is recommended to distinguish between FA and PT. This makes the diagnosis somewhat challenging, and it is not uncommon that the initial diagnostic impression is for an FA [13]. A study by Zmora et al [14] found that 63.6% of their cases had discordant results between the initial core needle biopsy and the final pathology report. In our case, the initial diagnosis was FA. Subsequently, the new biopsy made in our center concluded benign PT. Ultimately, the final pathology report was compatible with borderline PT.
PT is considered a de novo lesion that arises from periductal and lobular stroma. Multiple histological parameters are needed to classify PT into three distinct categories: benign, borderline, and malignant [15]. Benign PT represents 60-75% of all cases. Malignant PT constitutes 10-30% of all PT with an annual age-adjusted incidence of 2.1/1 million. The mean age of diagnosis of PT is 40 years old [16]. Meanwhile for the malignant subtype, it can range between 13 and 103 years, with a median of 50 years [17].
It is difficult to distinguish between the three subtypes due to tumor heterogeneity. In excised breasts, malignant PT is distinguished by nuclear pleomorphism, marked stromal overgrowth and > 10 mitosis per 10 high power field, among others. On the other hand, benign PT has few or no mitotic activity with no or mild stromal atypia. Borderline PT characteristics lie somewhere in between benign and malignant [16]. In our case the initial biopsy yielded benign PT, while the excised specimen concluded a borderline PT.
A study by Lae et al [18] discovered chromosome imbalances in 55% of 63 frozen samples of PT. Of these, gains in the 1q chromosome and 13q loss were associated with borderline and malignant grades. The authors suggested that PT can be classified into two genetically distinct groups: benign for those with no or few chromosome changes and malignant for those with recurrent chromosomal changes. We did not have access to chromosomal studies in our center, although we agree that performing one would be beneficial.
The malignant subtype seems even rarer in the pediatric and adolescent populations. In a single-center retrospective study of patients below 18 years old who underwent breast mass excision in a 9-year spawn found that 81.5% were FA, 3% were benign PT, with no malignant or borderline PT found [12]. At the time of this writing, there is no epidemiological data regarding this specific subtype in the children and adolescent age bracket. This is due to the limited number of series and cases reported.
Guidelines currently do not make a difference regarding treatment between adults and children [4]. The National Comprehensive Cancer Network (NCCN) guidelines recommend local excision with margins of 1 cm or more, with no axillary staging [19].
Recurrence, among other factors, is linked to the biological behavior of the tumor. It is reported that while up to 40% of malignant PT can recur, borderline and benign recurrence are at 32% and up to 25%, respectively. Most local recurrences occur within 2 years of the initial presentation [20]. Thus, distinguishing between the subtypes is considered important due to prognostic and treatment implications. A meta-analysis by Yu et al [6] concluded that some clinicopathological features are prognostic factors for recurrence. These factors included: moderate or severe stromal atypia and hypercellularity, stromal overgrowth, mitotic number of 5, tumor necrosis, tumor border, and margin status. Among the risk factors listed previously, our patient had none. At the time of this writing, 10 months have passed since the surgical intervention with no clinical signs of relapse.
Learning points
Attention is warranted when evaluating fast-growing breast masses in children and adolescents. It is essential to take PT into account. Treatment must be decided by a multidisciplinary team considering the size of the mass, the patient’s age, and the possible psychosocial repercussions.
Acknowledgments
We would like to thank Jesus Manuel Lozano-Garcia MD who inspired every one of us at Centro Oncologico Pediatrico to be a better healthcare professional and person.
Financial Disclosure
This research received no external funding.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Written informed consent was obtained from the patient’s mother prior to submitting this paper.
Author Contributions
Millan-Arreola, Lozano-Jaramillo and Tello de Meneses-Salazar conceived and conceptualized the idea. Lozano-Jaramillo, Esquer-Cota and Lavara-Miranda wrote the initial draft. Valenzuela-Espinoza and Millan-Arreola reviewed and edited the subsequent drafts. All authors helped with the visualization and have read and agreed to publish the final version of the manuscript.
Data Availability
The data used in this study were accurately cited within the manuscript. Further inquiries can be directed to the corresponding author.
Abbreviations
FA: fibroadenoma; FNB: fine needle biopsy; NCCN: National Comprehensive Cancer Network; NSAIDs: non-steroidal anti-inflammatory drugs; PBM: pediatric breast mass; PT: phyllodes tumor; WHO: World Health Organization
| References | ▴Top |
- Neinstein LS, Atkinson J, Diament M. Prevalence and longitudinal study of breast masses in adolescents. J Adolesc Health. 1993;14(4):277-281.
doi pubmed - Simmons PS, Jayasinghe YL, Wold LE, Melton LJ, 3rd. Breast carcinoma in young women. Obstet Gynecol. 2011;118(3):529-536.
doi pubmed pmc - Makhija D, Shah H, Bothra J, Jayaswal S. An adolescent with a phyllodes tumor: A case report and review. Int J Pediatr Adolesc Med. 2016;3(4):180-183.
doi pubmed pmc - Leraas HJ, Rosenberger LH, Ren Y, Ezekian B, Nag UP, Reed CR, Thomas SM, et al. Pediatric phyllodes tumors: A review of the National Cancer Data Base and adherence to NCCN guidelines for phyllodes tumor treatment. J Pediatr Surg. 2018;53(6):1123-1128.
doi pubmed - Tan PH, Ellis IO. Myoepithelial and epithelial-myoepithelial, mesenchymal and fibroepithelial breast lesions: updates from the WHO Classification of Tumours of the Breast 2012. J Clin Pathol. 2013;66(6):465-470.
doi pubmed - Yu CY, Huang TW, Tam KW. Management of phyllodes tumor: a systematic review and meta-analysis of real-world evidence. Int J Surg. 2022;107:106969.
doi pubmed - Xiao Y, Jiang Y, Xiong Y, Ruan S, Huang T. Pediatric malignant phyllodes tumors of the breast: characteristics and outcomes based on the surveillance epidemiology and end results database. J Surg Res. 2020;249:205-215.
doi pubmed - Hafeez S, Balarezo F, Ricci A, Jr. Benign phyllodes tumor in children: a study of 8 cases and review of the literature. J Pediatr Hematol Oncol. 2020;42(5):e388-e391.
doi pubmed - An adolescent with a phyllodes tumor: A case report and review of literature. ARC Journal of Pediatrics. 2019;5(2):1-3.
- Pistolese CA, Tanga I, Cossu E, Perretta T, Yamgoue M, Bonanno E, Simonetti G. A phyllodes tumor in a child. J Pediatr Adolesc Gynecol. 2009;22(3):e21-24.
doi pubmed - Knaus ME, Grabowksi JE. Pediatric breast masses: an overview of the subtypes, workup, imaging, and management. Adv Pediatr. 2021;68:195-209.
doi pubmed - McLaughlin CM, Gonzalez-Hernandez J, Bennett M, Piper HG. Pediatric breast masses: an argument for observation. J Surg Res. 2018;228:247-252.
doi pubmed - Lee AH, Hodi Z, Ellis IO, Elston CW. Histological features useful in the distinction of phyllodes tumour and fibroadenoma on needle core biopsy of the breast. Histopathology. 2007;51(3):336-344.
doi pubmed - Zmora O, Klin B, Iacob C, Meital A, Mendlovic S, Karni T. Characterizing excised breast masses in children and adolescents-Can a more aggressive pathology be predicted? J Pediatr Surg. 2020;55(10):2197-2200.
doi pubmed - Tan BY, Acs G, Apple SK, Badve S, Bleiweiss IJ, Brogi E, Calvo JP, et al. Phyllodes tumours of the breast: a consensus review. Histopathology. 2016;68(1):5-21.
doi pubmed pmc - Strode M, Khoury T, Mangieri C, Takabe K. Update on the diagnosis and management of malignant phyllodes tumors of the breast. Breast. 2017;33:91-96.
doi pubmed - Papas Y, Asmar AE, Ghandour F, Hajj I. Malignant phyllodes tumors of the breast: A comprehensive literature review. Breast J. 2020;26(2):240-244.
doi pubmed - Lae M, Vincent-Salomon A, Savignoni A, Huon I, Freneaux P, Sigal-Zafrani B, Aurias A, et al. Phyllodes tumors of the breast segregate in two groups according to genetic criteria. Mod Pathol. 2007;20(4):435-444.
doi pubmed - Ogunbiyi S, Perry A, Jakate K, Simpson J, George R. Phyllodes tumour of the breast and margins: How much is enough. Can J Surg. 2019;62(1):E19-E21.
doi pubmed pmc - Tse GM, Niu Y, Shi HJ. Phyllodes tumor of the breast: an update. Breast Cancer. 2010;17(1):29-34.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.


